Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
Mental health is a crucial aspect of our overall well-being, yet it is often overlooked and neglected. Fortunately, Medicare offers coverage for mental health services, but understanding what is covered can be confusing. In this article, we will explore the mental health services covered by Medicare and provide you with the information you need to make informed decisions about your mental health care. So, if you or a loved one is in need of mental health services, keep reading to learn more about what Medicare can do to help.
Medicare covers a range of mental health services, including outpatient counseling, therapy sessions, and inpatient psychiatric care. It also covers prescription drugs for mental health treatment. However, Medicare coverage for mental health services is subject to certain limitations and conditions. For instance, the beneficiary must have a diagnosed mental health condition, and the services must be provided by a qualified healthcare provider who accepts Medicare. Additionally, Medicare may only cover a certain number of sessions per year, depending on the type of service and the provider’s recommendation.
Contents
- Understanding Mental Health Services Covered by Medicare
- Frequently Asked Questions
- What mental health services does Medicare cover?
- How do I know if I’m eligible for Medicare mental health services?
- What costs are associated with Medicare mental health services?
- What mental health conditions are covered by Medicare?
- How do I find a qualified healthcare provider who accepts Medicare for mental health services?
- Medicare Behavioral Health Coverage
Understanding Mental Health Services Covered by Medicare
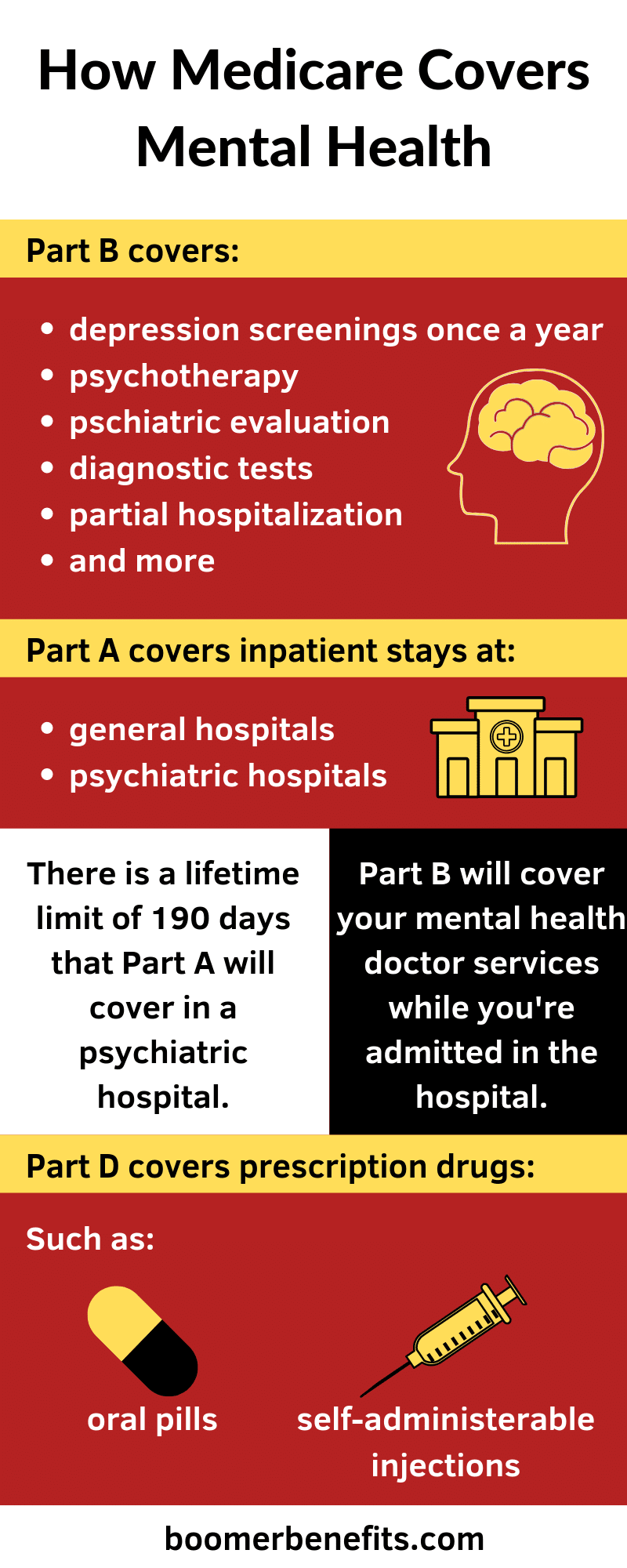
Mental health is an essential aspect of overall health, and Medicare has taken a significant step towards ensuring that beneficiaries can access mental health services. Mental health services are covered under Medicare Part B, which is considered the medical insurance aspect of Medicare. This article aims to provide detailed information on the mental health services that Medicare covers.
Outpatient Mental Health Services
Medicare covers a range of outpatient mental health services, including individual and group psychotherapy sessions. It also covers diagnostic assessments, psychiatric evaluations, and medication management services. Medicare also allows for a maximum of 80% of the Medicare-approved amount for mental health services.
In addition, Medicare covers partial hospitalization programs, which are structured treatment programs that provide intensive psychiatric treatment while allowing patients to live at home. Partial hospitalization programs are ideal for individuals who require more intensive treatment than outpatient services but do not require hospitalization.
Inpatient Mental Health Services
Medicare covers inpatient mental health services, including psychiatric hospitalization and psychiatric nursing care. Medicare Part A covers psychiatric hospitalization, including room, board, and services provided by the hospital. However, Medicare only covers up to 190 days of inpatient psychiatric hospitalization over a person’s lifetime.
In addition, Medicare also covers inpatient psychiatric nursing care in a skilled nursing facility. This is suitable for individuals who require psychiatric nursing care but do not require hospitalization.
Telehealth Services
Medicare covers telehealth services for mental health, which allows beneficiaries to receive mental health services from the comfort of their homes. Telehealth services include psychotherapy, medication management, and psychiatric evaluations.
Telehealth services are ideal for individuals who live in rural areas or have limited access to mental health services. Medicare covers telehealth services, but the beneficiary must have a secure internet connection and access to a computer or smartphone.
Intensive Outpatient Programs
Medicare covers intensive outpatient programs, which are structured treatment programs that provide intensive psychiatric treatment while allowing patients to live at home. Intensive outpatient programs are suitable for individuals who require more intensive treatment than outpatient services but do not require hospitalization.
Intensive outpatient programs typically include group therapy, individual therapy, and medication management services. Medicare covers 80% of the Medicare-approved amount for intensive outpatient programs.
Screening for Depression and Alcohol Misuse
Medicare covers screening for depression and alcohol misuse as part of its preventive services. This means that beneficiaries can receive screening for depression and alcohol misuse at no cost to them.
Screening for depression and alcohol misuse is essential because it enables early detection, which can lead to early intervention and treatment.
Benefits of Medicare Mental Health Coverage
One of the significant benefits of Medicare mental health coverage is that it provides beneficiaries with access to mental health services. This means that individuals who require mental health services can receive them without worrying about the cost.
In addition, Medicare mental health coverage includes a range of services, from outpatient services to inpatient hospitalization. This means that beneficiaries can receive the level of care that they require.
Limitations of Medicare Mental Health Coverage
Medicare mental health coverage has some limitations. For example, Medicare only covers up to 80% of the Medicare-approved amount for mental health services. Beneficiaries are responsible for paying the remaining 20%.
In addition, Medicare only covers up to 190 days of inpatient psychiatric hospitalization over a person’s lifetime. This means that beneficiaries who require more than 190 days of inpatient psychiatric hospitalization will be responsible for the cost.
Medicare vs. Private Insurance
Medicare mental health coverage is comparable to private insurance coverage. However, private insurance coverage may provide more extensive coverage than Medicare.
For example, private insurance may cover more than 190 days of inpatient psychiatric hospitalization. Private insurance may also have lower copayments and deductibles for mental health services.
Conclusion
In conclusion, Medicare provides beneficiaries with access to mental health services. It covers a range of services, from outpatient services to inpatient hospitalization. Medicare also covers telehealth services and screening for depression and alcohol misuse.
However, Medicare mental health coverage has some limitations, such as only covering up to 80% of the Medicare-approved amount for mental health services. Beneficiaries who require more than 190 days of inpatient psychiatric hospitalization will be responsible for the cost.
Frequently Asked Questions
What mental health services does Medicare cover?
Medicare covers a range of mental health services for individuals who need treatment for mental health conditions. These services include counseling and therapy sessions, psychiatric evaluations, and medication management. Medicare also covers inpatient psychiatric care in a hospital or specialized psychiatric facility.
It’s important to note that Medicare may only cover mental health services that are deemed medically necessary. This means that the service must be required to diagnose or treat a mental health condition. Additionally, there may be limitations on the number of visits or types of services that are covered, so it’s important to check with your healthcare provider and Medicare plan to understand your coverage.
How do I know if I’m eligible for Medicare mental health services?
To be eligible for Medicare mental health services, you must be enrolled in Medicare Part B. This includes individuals who are 65 years or older, as well as those who are younger than 65 years old but have a qualifying disability.
Once enrolled in Medicare Part B, you can receive mental health services from any qualified healthcare provider who accepts Medicare. It’s important to note that some mental health services may require a referral from your primary care physician or a specialist, so it’s important to discuss your treatment plan with your healthcare provider.
What costs are associated with Medicare mental health services?
The cost of Medicare mental health services may vary depending on the service and the healthcare provider. Generally, Medicare covers 80% of the cost of mental health services, and you are responsible for the remaining 20%. However, if you have a Medicare supplemental insurance plan, it may cover some or all of the remaining costs.
It’s important to note that some mental health services may have deductibles or co-payments that apply. Additionally, there may be limits on the number of visits or services that are covered, so it’s important to check with your healthcare provider and Medicare plan to understand your coverage.
What mental health conditions are covered by Medicare?
Medicare covers a range of mental health conditions, including depression, anxiety, bipolar disorder, schizophrenia, and other serious mental illnesses. Additionally, Medicare covers mental health services that are required for the treatment of substance use disorders.
To be eligible for Medicare mental health services, the condition must be diagnosed by a qualified healthcare provider and deemed medically necessary. Your healthcare provider can work with you to develop a treatment plan that is tailored to your specific mental health condition.
How do I find a qualified healthcare provider who accepts Medicare for mental health services?
To find a qualified healthcare provider who accepts Medicare for mental health services, you can use the Medicare Physician Compare tool on the Medicare website. This tool allows you to search for healthcare providers by location, specialty, and other criteria.
You can also contact your local Medicare office or healthcare provider to get a list of qualified mental health providers in your area. It’s important to choose a healthcare provider who is experienced in treating your specific mental health condition and who accepts Medicare to ensure that you receive the best possible care.
Medicare Behavioral Health Coverage
In conclusion, Medicare provides coverage for a range of mental health services, including counseling, therapy, and medication management. These services can be accessed by those who meet the eligibility requirements and have a mental health diagnosis. However, it is important to note that some services may require a co-payment or deductible, and there may be limits on the number of visits or types of services covered.
Despite these limitations, Medicare coverage for mental health services is an important step towards ensuring that individuals receive the care they need to manage their mental health conditions. By seeking out the appropriate services and working with qualified mental health professionals, beneficiaries can access the support and treatment necessary to improve their well-being and quality of life.
Overall, the availability of mental health services through Medicare is an important resource for those struggling with mental health issues. By taking advantage of these services, individuals can receive the care they need to manage their conditions and live healthy, fulfilling lives.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts