Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
Medicare is a federal health insurance program that covers most people over the age of 65, as well as those with certain disabilities or medical conditions. One of the most common questions Medicare beneficiaries have is how long the program will pay for their rehabilitation services. While there is no one-size-fits-all answer, understanding Medicare’s coverage rules and limitations can help you plan for your recovery with confidence.
Rehabilitation can be a critical component of recovery after an illness, injury, or surgery. But how many days will Medicare pay for rehab? The answer depends on several factors, including the type of rehabilitation you need, your medical condition, and the specific Medicare plan you have. In this article, we’ll explore some of the key things you need to know about Medicare’s coverage for rehabilitation services, so you can make informed decisions about your healthcare needs.
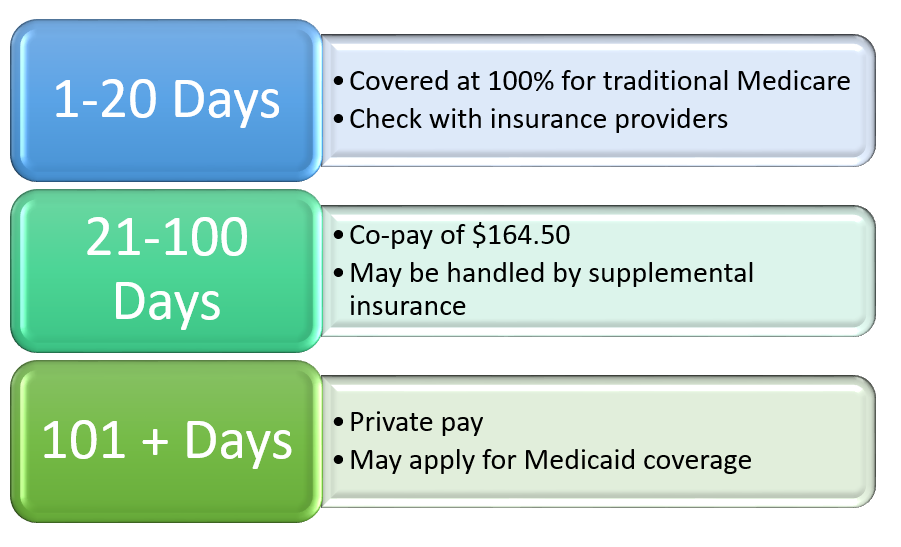
Medicare covers up to 100 days of inpatient rehabilitation care per benefit period. However, there are certain requirements that must be met to qualify for coverage. The first 20 days are fully covered, but a daily coinsurance amount is required for days 21-100. If you need more than 100 days of rehab, you may be responsible for all costs. It is important to check with your healthcare provider and Medicare for specific details and coverage options.
How Many Days Will Medicare Pay for Rehab?
Medicare is a federal health insurance program that covers people who are 65 or older, people with disabilities, and people with End-Stage Renal Disease (ESRD). Medicare covers a variety of healthcare services, including hospital stays, doctor visits, and rehabilitation services. But how many days will Medicare pay for rehab? Let’s find out.
1. Inpatient Rehabilitation Facility (IRF)
Inpatient Rehabilitation Facility (IRF) is a type of rehabilitation facility where patients stay overnight and receive intensive rehabilitation services. Medicare will cover up to 90 days of inpatient rehab care per benefit period. However, if the patient needs more than 90 days of care, Medicare may cover additional days if the patient’s condition continues to improve.
To qualify for IRF, the patient must have a doctor’s order for inpatient rehab care, require at least three hours of intensive rehab services per day, and have a condition that requires intensive rehab services.
2. Skilled Nursing Facility (SNF)
Skilled Nursing Facility (SNF) is a type of rehabilitation facility where patients receive rehabilitation services, such as physical therapy, occupational therapy, and speech-language pathology. Medicare will cover up to 100 days of SNF care per benefit period.
To qualify for SNF, the patient must have a qualifying hospital stay of at least three days, require skilled nursing care or skilled rehabilitation services, and have a condition that requires daily skilled care.
3. Outpatient Rehabilitation
Outpatient rehabilitation services are provided in a clinic or hospital setting. Medicare will cover outpatient rehabilitation services, such as physical therapy, occupational therapy, and speech-language pathology, as long as the services are medically necessary.
There is no limit on the number of outpatient rehabilitation services that Medicare will cover. However, the patient may be responsible for a co-payment or co-insurance for each service.
4. Home Health Care
Home health care is a type of rehabilitation service that is provided in the patient’s home. Medicare will cover home health care services, such as physical therapy, occupational therapy, and speech-language pathology, as long as the services are medically necessary.
Medicare will cover up to 100 days of home health care per benefit period. However, the patient must be homebound and require skilled care to qualify for home health care.
5. Hospice Care
Hospice care is a type of care that is provided to terminally ill patients who have a life expectancy of six months or less. Medicare will cover hospice care services, such as pain management, nursing care, and social services.
Hospice care services are covered for as long as the patient continues to meet the eligibility criteria. However, the patient must give up curative treatment to qualify for hospice care.
6. Durable Medical Equipment (DME)
Durable Medical Equipment (DME) is equipment that is used to treat or prevent a medical condition, such as a wheelchair, oxygen equipment, or a hospital bed. Medicare will cover DME as long as the equipment is medically necessary.
There is no limit on the amount of DME that Medicare will cover. However, the patient may be responsible for a co-payment or co-insurance for each piece of equipment.
7. Prosthetic Devices
Prosthetic devices are devices that are used to replace a missing body part, such as a prosthetic limb or a prosthetic eye. Medicare will cover prosthetic devices as long as the device is medically necessary.
There is no limit on the amount of prosthetic devices that Medicare will cover. However, the patient may be responsible for a co-payment or co-insurance for each device.
8. Mental Health Services
Medicare will cover mental health services, such as counseling and psychotherapy, as long as the services are medically necessary. There is no limit on the number of mental health services that Medicare will cover.
However, the patient may be responsible for a co-payment or co-insurance for each service.
9. Preventive Services
Medicare will cover preventive services, such as annual wellness visits, flu shots, and mammograms, as long as the services are medically necessary. There is no limit on the number of preventive services that Medicare will cover.
However, the patient may be responsible for a co-payment or co-insurance for each service.
10. Prescription Drugs
Medicare will cover prescription drugs under Part D of the program. The coverage and cost of the drugs vary depending on the specific drug and the patient’s plan. The patient may be responsible for a monthly premium, deductible, co-payment, or co-insurance for each prescription drug.
In conclusion, Medicare will cover a variety of rehabilitation services, including inpatient rehab, skilled nursing care, outpatient rehab, home health care, hospice care, DME, prosthetic devices, mental health services, preventive services, and prescription drugs. The coverage and cost of the services may vary depending on the specific service and the patient’s plan. It’s important to understand the coverage and eligibility criteria before seeking any rehabilitation services.
Contents
- Frequently Asked Questions
- How Many Days Will Medicare Pay for Rehab?
- What Types of Rehabilitative Services Are Covered by Medicare?
- Do I Need a Referral from My Doctor to Receive Rehabilitative Services?
- Can I Receive Rehabilitation Services from a Non-Medicare Approved Provider?
- What Happens if My Medicare Coverage for Rehabilitation Services Runs Out?
- Will Medicare pay for rehab?
Frequently Asked Questions
How Many Days Will Medicare Pay for Rehab?
Medicare covers a certain number of days for rehabilitation services. The number of days covered by Medicare depends on the type of rehabilitation service needed and the individual’s medical condition. For inpatient rehabilitation services, Medicare will cover up to 100 days per benefit period. However, this coverage is subject to certain conditions, such as the individual’s need for daily skilled care and progress in their rehabilitation goals.
For outpatient rehabilitation services, Medicare will cover an unlimited number of sessions as long as the services are medically necessary and provided by a Medicare-approved provider. It’s important to note that the individual may be responsible for paying a portion of the cost of rehabilitation services, such as coinsurance or deductibles.
What Types of Rehabilitative Services Are Covered by Medicare?
Medicare covers a variety of rehabilitative services, including physical therapy, occupational therapy, and speech-language pathology services. These services are covered when they are deemed medically necessary to improve the individual’s condition, function, or quality of life. Medicare also covers inpatient rehabilitation services provided in a hospital or skilled nursing facility, as well as outpatient rehabilitation services provided in a physician’s office or clinic.
It’s important to note that not all rehabilitation services are covered by Medicare. For example, Medicare does not cover services that are not considered medically necessary, such as services for general health and fitness or cosmetic purposes. It’s important to check with Medicare or a healthcare provider to determine the specific services that are covered under the individual’s plan.
Do I Need a Referral from My Doctor to Receive Rehabilitative Services?
In most cases, a referral from a doctor is required to receive rehabilitative services covered by Medicare. The referral must come from a doctor or healthcare provider who is enrolled in Medicare and must specify the type and frequency of the services needed. The referral must also be made before the services are provided.
In some cases, the individual may be able to self-refer for certain types of rehabilitative services, such as physical therapy for a limited number of sessions. However, it’s important to check with Medicare or a healthcare provider to determine the specific requirements for self-referral.
Can I Receive Rehabilitation Services from a Non-Medicare Approved Provider?
In general, Medicare will only cover rehabilitative services provided by a Medicare-approved provider. This means that the provider must meet certain qualifications and standards set by Medicare in order to be eligible for reimbursement. These standards include requirements for licensure, accreditation, and quality of care.
However, there may be some exceptions to this rule. In certain situations, Medicare may cover services provided by a non-Medicare approved provider if the provider is the only one available in the area or if the individual has a religious or cultural objection to receiving services from a Medicare-approved provider. It’s important to check with Medicare or a healthcare provider to determine the specific requirements for receiving services from a non-Medicare approved provider.
What Happens if My Medicare Coverage for Rehabilitation Services Runs Out?
If the individual’s Medicare coverage for rehabilitation services runs out, they may be responsible for paying for the services out of pocket. However, there may be other options available to help cover the cost of rehabilitation services, such as private insurance or Medicaid.
It’s important to note that the individual may be able to appeal a decision to end their Medicare coverage for rehabilitation services if they feel that they still need the services to improve their condition. An appeal can be made by filing a request for a reconsideration with the Medicare Administrative Contractor (MAC) within 120 days of receiving the notice of the decision.
Will Medicare pay for rehab?
In conclusion, the number of days that Medicare will pay for rehab depends on different factors. These factors include the type of rehab service needed, the type of Medicare plan you have, and the progress you are making in your rehab program. It is important to keep in mind that while Medicare may cover a certain number of days for rehab, it is ultimately up to your healthcare provider to determine the appropriate length of treatment.
It is also important to note that if you require additional rehab services beyond what Medicare covers, you may be responsible for paying for those services out of pocket. It is therefore essential to understand your Medicare coverage and to discuss any concerns or questions you may have with your healthcare provider.
Overall, understanding your Medicare coverage for rehab services is crucial to ensure that you receive the care you need. By working closely with your healthcare provider and staying informed about your coverage, you can make informed decisions about your rehab treatment and achieve the best possible outcomes.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts