Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
Medicare is a government-funded healthcare program that provides coverage to millions of Americans. One of the benefits of this program is rehabilitation services for those who need them. However, many people are unsure of how long Medicare will pay for rehab. In this article, we will explore the details of Medicare coverage for rehabilitation services and answer the question, “How many days does Medicare pay for rehab?”
Rehabilitation is an essential component of many healthcare plans, and Medicare recognizes this importance. However, it’s crucial to understand the limitations and rules surrounding Medicare coverage for rehab. Whether you or a loved one needs rehab services, understanding what Medicare covers can help you make informed decisions and ease the financial burden. So, let’s dive into the details and find out how many days Medicare pays for rehab.
How Many Days Does Medicare Pay for Rehab?
Medicare provides coverage for various types of rehabilitation services. However, the duration of coverage depends on the type of rehab service and the patient’s medical condition. In this article, we will discuss the number of days that Medicare pays for rehab services.
Inpatient Rehabilitation Facility (IRF) Services
An Inpatient Rehabilitation Facility (IRF) is a hospital that specializes in providing intensive rehabilitation services to patients with complex medical conditions. Medicare covers up to 90 days of inpatient rehabilitation services in an IRF. After the initial 90-day period, Medicare will pay for an additional 60 days of care, but the patient is responsible for paying a daily coinsurance fee.
During the initial 90-day period, Medicare covers all necessary services, including room and board, nursing care, physical therapy, occupational therapy, speech-language pathology, and social services. However, the patient must meet certain criteria to qualify for IRF services, such as having a condition that requires multiple types of therapy or needing at least three hours of therapy per day.
Benefits of Inpatient Rehabilitation Facility Services
- Intensive therapy services
- 24-hour medical care and supervision
- Individualized treatment plans
- Access to specialized equipment and resources
IRF Services vs. Skilled Nursing Facility Services
| IRF Services | Skilled Nursing Facility Services |
|---|---|
| Intensive therapy services | Less intensive therapy services |
| 24-hour medical care and supervision | Less medical care and supervision |
| Individualized treatment plans | Less individualized treatment plans |
| Access to specialized equipment and resources | Less access to specialized equipment and resources |
Outpatient Rehabilitation Services
Outpatient rehabilitation services refer to therapy services provided on an outpatient basis, meaning the patient does not stay overnight at a hospital or facility. Medicare covers outpatient rehabilitation services, including physical therapy, occupational therapy, and speech-language pathology, as long as the services are medically necessary.
Medicare covers 80% of the approved amount for outpatient rehabilitation services, and the patient is responsible for the remaining 20%. There is no limit to the number of outpatient rehabilitation services that Medicare covers.
Benefits of Outpatient Rehabilitation Services
- Less expensive than inpatient rehabilitation services
- Flexibility in scheduling therapy sessions
- Ability to receive therapy services at home
- Less disruptive to daily life
Outpatient Rehabilitation Services vs. Inpatient Rehabilitation Facility Services
| Outpatient Rehabilitation Services | Inpatient Rehabilitation Facility Services |
|---|---|
| Less expensive than inpatient rehabilitation services | More expensive than outpatient rehabilitation services |
| Flexibility in scheduling therapy sessions | Structured therapy schedule |
| Ability to receive therapy services at home | Must stay at hospital or facility |
| Less disruptive to daily life | More disruptive to daily life |
Home Health Services
Home health services refer to medical services provided in the patient’s home. Medicare covers home health services, including physical therapy, occupational therapy, and speech-language pathology, as long as the services are medically necessary.
Medicare covers home health services for as long as the patient needs them, and there is no limit to the number of services that Medicare covers. However, the patient must meet certain criteria to qualify for home health services, such as being homebound and needing intermittent skilled nursing care or therapy services.
Benefits of Home Health Services
- Ability to receive therapy services at home
- Less disruptive to daily life
- Individualized treatment plans
- Access to specialized equipment and resources
Home Health Services vs. Outpatient Rehabilitation Services
| Home Health Services | Outpatient Rehabilitation Services |
|---|---|
| Ability to receive therapy services at home | Must go to a hospital or facility for therapy services |
| Less disruptive to daily life | Requires leaving home for therapy services |
| Individualized treatment plans | May not be as individualized as home health services |
| Access to specialized equipment and resources | May not have access to specialized equipment and resources |
Conclusion
Medicare provides coverage for various types of rehabilitation services, including inpatient rehabilitation facility services, outpatient rehabilitation services, and home health services. The duration of coverage depends on the type of rehab service and the patient’s medical condition. Patients should consult with their healthcare providers to determine the best type of rehab service for their individual needs.
Contents
- Frequently Asked Questions
- Q: How many days does Medicare pay for rehab?
- Q: What is a benefit period in Medicare?
- Q: Does Medicare cover outpatient rehab services?
- Q: How much will I have to pay for rehab services under Medicare?
- Q: Can I receive rehab services outside of a hospital or SNF under Medicare?
- Will Medicare pay for rehab?
Frequently Asked Questions
Q: How many days does Medicare pay for rehab?
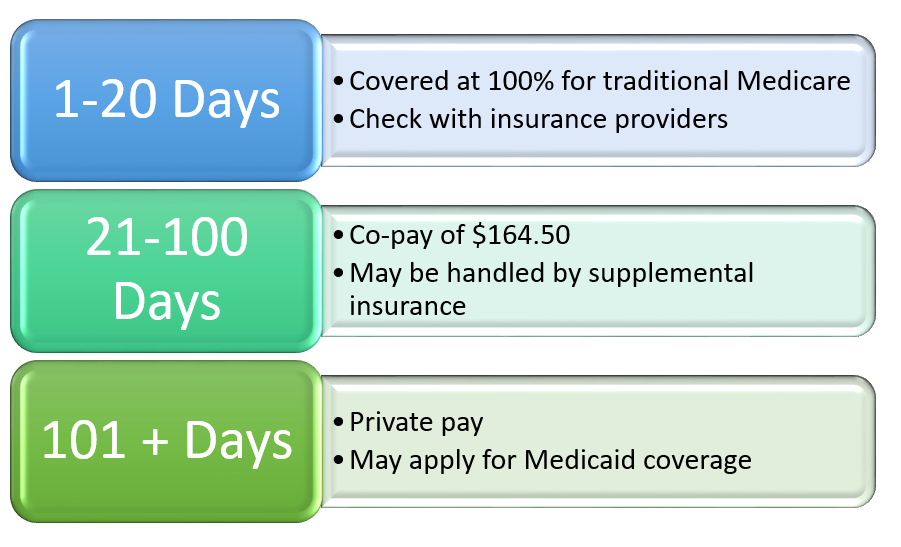
Medicare will pay for up to 100 days of skilled nursing facility (SNF) care per benefit period. However, the amount of coverage provided depends on the type of Medicare plan you have. Medicare Part A covers inpatient hospital stays, including SNF care, while Medicare Part B covers outpatient therapy services.
It’s important to note that Medicare will only cover rehab services that are deemed medically necessary and ordered by a doctor. Additionally, there are certain criteria that must be met in order for Medicare to continue paying for SNF care beyond the initial 20 days. If you have questions about your specific Medicare coverage for rehab, it’s best to contact your plan provider directly.
Q: What is a benefit period in Medicare?
A benefit period in Medicare begins the day you are admitted to a hospital or SNF and ends when you have gone 60 consecutive days without receiving any hospital or SNF care. During each benefit period, you are eligible for a set amount of coverage for various healthcare services.
For example, Medicare Part A covers inpatient hospital stays for up to 90 days per benefit period. Once you have used up your allotted coverage for a particular service, you must wait until the start of a new benefit period to receive additional coverage. It’s important to understand your benefit period and coverage limits to avoid unexpected medical bills.
Q: Does Medicare cover outpatient rehab services?
Yes, Medicare Part B covers outpatient rehab services, including physical therapy, occupational therapy, and speech therapy. However, there may be certain limitations on coverage, such as the number of therapy sessions allowed per year.
In order for Medicare to cover outpatient rehab services, they must be deemed medically necessary and ordered by a doctor. Your doctor will also need to provide regular updates on your progress to ensure that the therapy is still needed and effective.
Q: How much will I have to pay for rehab services under Medicare?
The amount you will have to pay for rehab services under Medicare depends on several factors, including the type of service, the setting in which it is provided, and your specific Medicare plan.
For inpatient rehab services provided in a SNF, Medicare Part A covers the first 20 days at 100% and a portion of the cost for days 21-100. After day 100, you will be responsible for all costs. For outpatient rehab services provided under Medicare Part B, you will generally be responsible for a 20% coinsurance after meeting your annual deductible.
Q: Can I receive rehab services outside of a hospital or SNF under Medicare?
Yes, Medicare also covers home health services, which can include rehab services provided in your own home. However, there are certain criteria that must be met in order to qualify for home health services, such as being homebound and needing skilled nursing care or therapy services.
In some cases, Medicare may also cover rehab services provided in an outpatient setting, such as a rehabilitation center or clinic. It’s important to check with your Medicare plan provider to understand your specific coverage for rehab services outside of a hospital or SNF.
Will Medicare pay for rehab?
In conclusion, Medicare is a valuable resource for those in need of rehab services. While the number of days covered varies depending on the type of rehab and individual circumstances, it is important to know that Medicare can provide a significant amount of coverage. It is crucial to work with healthcare providers and Medicare representatives to determine the best plan of action for your specific needs.
Remember, Medicare is designed to help individuals achieve better health outcomes and regain their independence. By utilizing the resources available, you can take the first step towards a healthier and happier life. Don’t hesitate to explore your options and take advantage of the benefits that Medicare has to offer.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts