Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
As we age, our bodies may require additional medical assistance to maintain our health. One common medical device that older adults may need is a catheter. If you or a loved one is on Medicare, you may wonder how many catheters Medicare will pay for per month.
Understanding Medicare’s coverage for catheters can be confusing, but it’s important to know the limits and guidelines to ensure you receive the appropriate care. In this article, we’ll explore the details of Medicare’s catheter coverage and provide helpful information for those who may need this medical device.
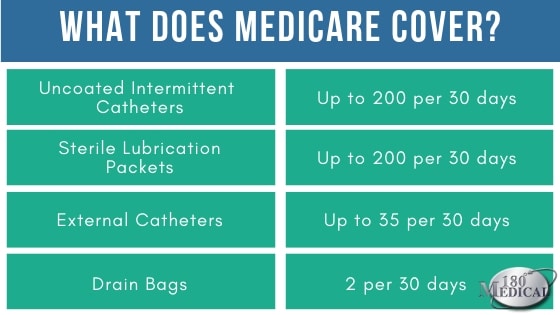
Medicare Part B covers up to 200 disposable catheters per month if you have a medical need for them. If you need more than 200 catheters per month, you may be able to get an exception. You can talk to your doctor or supplier about getting an exception to the Medicare coverage limit.
How Many Catheters Will Medicare Pay for Per Month?
If you or someone you care for is living with a medical condition that requires the use of catheters, you may be wondering how many catheters Medicare will pay for per month. The answer to this question can vary depending on a number of factors, including the type of catheters needed and the specific Medicare plan in question. In this article, we’ll explore some of the key considerations related to Medicare coverage for catheters and help you better understand how to navigate the process of securing the care you need.
Understanding Medicare Coverage for Catheters
Medicare is a federal health insurance program that provides coverage for a wide range of medical services, including catheters. However, the specifics of this coverage can vary depending on the individual plan and the particular type of catheters needed. In general, Medicare will cover catheters that are deemed medically necessary by a healthcare provider. This can include intermittent catheters, which are used to empty the bladder, and external catheters, which are used to collect urine.
The number of catheters that Medicare will cover per month can vary depending on the individual’s medical needs and the specifics of their Medicare plan. Some plans may limit the number of catheters that are covered per month, while others may cover an unlimited number of catheters. It’s important to understand the specifics of your Medicare plan and work closely with your healthcare provider to ensure that you have access to the care you need.
Factors That Can Affect Medicare Coverage for Catheters
While Medicare does provide coverage for catheters, there are a number of factors that can impact the specifics of this coverage. Some of the key factors to keep in mind include:
1. Type of Catheter: Medicare may provide coverage for different types of catheters, including intermittent and external catheters. The specific type of catheter needed can impact the amount of coverage provided.
2. Medical Necessity: In order for Medicare to provide coverage for catheters, they must be deemed medically necessary by a healthcare provider. This determination can impact the number of catheters that are covered per month.
3. Medicare Plan: The specifics of your Medicare plan can impact the amount of coverage provided for catheters. Some plans may cover an unlimited number of catheters per month, while others may have limits in place.
4. Prescription Requirements: In some cases, Medicare may require a prescription for catheters in order to provide coverage. It’s important to work closely with your healthcare provider to ensure that you have access to the care you need.
Benefits of Medicare Coverage for Catheters
While navigating the specifics of Medicare coverage for catheters can be challenging, there are a number of benefits to having this coverage in place. Some of the key benefits include:
1. Access to Care: Medicare coverage can provide access to the care and supplies needed to manage a medical condition that requires the use of catheters.
2. Financial Assistance: Medicare coverage for catheters can help offset the cost of these supplies, making them more affordable for individuals and families.
3. Peace of Mind: Knowing that Medicare provides coverage for catheters can provide peace of mind and help alleviate some of the stress associated with managing a medical condition.
Catheter Types and Medicare Coverage
As mentioned earlier, the type of catheter needed can impact the specifics of Medicare coverage. Here’s a closer look at some of the most common types of catheters and how they are covered by Medicare:
1. Intermittent Catheters: These catheters are used to empty the bladder and are typically covered by Medicare. The number of catheters covered per month can vary depending on the individual’s medical needs and the specifics of their Medicare plan.
2. External Catheters: These catheters are used to collect urine and are also typically covered by Medicare. As with intermittent catheters, the number of external catheters covered per month can vary depending on the individual’s medical needs and the specifics of their Medicare plan.
3. Foley Catheters: Foley catheters are typically used in hospital or nursing home settings and may be covered by Medicare in certain situations. However, coverage for these catheters is typically more limited than coverage for intermittent or external catheters.
Catheter Use and Care
In addition to understanding the specifics of Medicare coverage for catheters, it’s also important to know how to properly use and care for these medical devices. Here are a few key tips to keep in mind:
1. Cleanliness is Key: Proper hygiene is essential when using catheters. Be sure to wash your hands thoroughly before and after handling catheters, and follow all cleaning and sterilization instructions provided by your healthcare provider.
2. Proper Insertion: Proper insertion of catheters can help minimize discomfort and reduce the risk of infection. Be sure to work closely with your healthcare provider to ensure that you are properly inserting and removing your catheters.
3. Storage and Disposal: Proper storage and disposal of catheters is also important. Be sure to store catheters in a clean, dry place and dispose of used catheters in accordance with all local regulations.
Catheters: Medicare vs. Private Insurance
While Medicare provides coverage for catheters, it’s important to note that private insurance plans may also offer coverage for these medical devices. In some cases, private insurance may offer more comprehensive coverage or may cover a wider range of catheter types. Be sure to compare the specifics of your Medicare plan to any private insurance coverage you may have to determine which option is best for your individual needs.
Catheter Supplies: Where to Find Them
If you need catheters to manage a medical condition, there are a number of resources available to help you find the supplies you need. Some of the most common places to find catheter supplies include:
1. Medical Supply Companies: There are a number of medical supply companies that specialize in providing catheter supplies to individuals and healthcare providers.
2. Healthcare Providers: Your healthcare provider may be able to provide you with information or resources related to catheter supplies.
3. Medicare: If you have Medicare coverage, be sure to explore the options available through your plan to find the catheter supplies you need.
Conclusion
Navigating Medicare coverage for catheters can be challenging, but understanding the specifics of your plan and working closely with your healthcare provider can help ensure that you have access to the care you need. Whether you are using intermittent catheters, external catheters, or another type of catheter, proper use and care are essential for managing your medical condition. With the right resources and support, you can find the catheter supplies you need to live your best life.
Contents
- Frequently Asked Questions
- How Many Catheters Will Medicare Pay for Per Month?
- Do I Need a Prescription for Medicare to Cover My Catheters?
- What Types of Catheters Does Medicare Cover?
- Do I Have to Use a Medicare-Approved Catheter Supplier?
- What Should I Do if I Have Trouble Getting My Catheters Covered by Medicare?
- How much do catheters cost?
Frequently Asked Questions
As a professional writer, I have researched and compiled the following frequently asked questions and answers about Medicare coverage of catheters.
How Many Catheters Will Medicare Pay for Per Month?
Medicare covers up to 200 intermittent catheters per month, depending on the patient’s medical condition and needs. Intermittent catheters are used for draining the bladder and are considered medically necessary for people with conditions such as spinal cord injuries, multiple sclerosis, and spina bifida.
However, if a patient requires more than 200 catheters per month, they may be eligible for additional coverage through Medicare. In these cases, a healthcare provider must submit a request for additional coverage and provide documentation of the patient’s medical necessity for the additional catheters.
Do I Need a Prescription for Medicare to Cover My Catheters?
Yes, a prescription from a healthcare provider is required for Medicare to cover catheters. The prescription must specify the type and quantity of catheters needed, as well as the frequency of use. It is important to keep the prescription on file and provide it to the catheter supplier when ordering supplies.
In addition, Medicare requires that the catheter supplier be enrolled in Medicare in order to be eligible for coverage. Patients should always verify that their supplier is enrolled in Medicare and that they are not responsible for any out-of-pocket costs before ordering catheters.
What Types of Catheters Does Medicare Cover?
Medicare covers a variety of catheter types, including intermittent catheters, indwelling catheters, and external catheters. Intermittent catheters are the most commonly covered type and are used for draining the bladder. Indwelling catheters are inserted into the bladder and are left in place for a longer period of time. External catheters, also known as condom catheters, are placed over the penis and are used for male patients who are unable to use other types of catheters.
It is important to note that Medicare may only cover certain types of catheters for certain medical conditions. Patients should consult with their healthcare provider to determine the appropriate catheter type for their specific needs.
Do I Have to Use a Medicare-Approved Catheter Supplier?
While it is recommended that patients use a Medicare-approved catheter supplier, it is not required. However, using a non-approved supplier may result in the patient being responsible for some or all of the cost of the catheters. It is important to verify that the supplier is enrolled in Medicare before ordering supplies to ensure that they are eligible for coverage.
If a patient chooses to use a non-approved supplier, they should keep all receipts and documentation of the purchase in case they need to submit a claim for reimbursement.
What Should I Do if I Have Trouble Getting My Catheters Covered by Medicare?
If a patient has trouble getting their catheters covered by Medicare, they should first contact their catheter supplier to verify that they are enrolled in Medicare and that the patient is not responsible for any out-of-pocket costs. If the issue persists, the patient should contact Medicare directly to inquire about the coverage policy and to file a complaint if necessary.
Patients may also consult with a healthcare advocate or an attorney who specializes in Medicare coverage to help navigate the system and ensure that they receive the coverage they are entitled to.
How much do catheters cost?
In conclusion, determining how many catheters Medicare will pay for per month can be a complex and confusing process. However, with the right information and guidance, patients can navigate the system to ensure they receive the necessary supplies for their medical needs.
It is crucial to work with a healthcare provider and supplier that has experience dealing with Medicare coverage. They can help patients understand their options and provide guidance on how to obtain the necessary documentation and prescriptions.
Ultimately, patients should not be afraid to advocate for themselves and their medical needs. By staying informed and proactive, they can ensure they receive the appropriate number of catheters each month and maintain their health and well-being.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts