Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
Medicare is a federal health insurance program that provides coverage for millions of Americans, including those who require rehabilitation services. However, many people are unclear about how long Medicare will pay for rehabilitation and what types of services are covered.
If you or a loved one is in need of rehabilitation, it is important to understand the guidelines and limitations of Medicare coverage. In this article, we will explore the duration of Medicare coverage for rehabilitation services, the types of services that are covered, and what you can do if your coverage runs out. So, let’s dive in and learn more about Medicare and rehabilitation.
How Long Does Medicare Pay for Rehabilitation?
Rehabilitation is an important aspect of healthcare for seniors, as it helps them recover from injuries or illnesses and improve their quality of life. Medicare is a federal health insurance program that covers rehabilitation services, but many seniors are unsure about how long they can receive this coverage. In this article, we will explore how long Medicare pays for rehabilitation and what services are covered.
Medicare Coverage for Rehabilitation
Medicare covers a wide range of rehabilitation services for individuals who have a medical need for them. These services may include physical therapy, occupational therapy, and speech-language pathology services. Medicare Part B covers outpatient rehabilitation services, while Medicare Part A covers inpatient rehabilitation services.
If you require rehabilitation services, your healthcare provider will create a plan of care that outlines the services you need and for how long you will need them. This plan should be reviewed regularly to ensure that you are receiving the appropriate level of care.
Medicare Coverage Limits for Rehabilitation
While Medicare does cover rehabilitation services, there are limits to how much coverage you can receive. For outpatient rehabilitation services, Medicare will cover up to $2,110 per year. This amount may be adjusted each year, so it is important to check with Medicare to see what the current limits are.
For inpatient rehabilitation services, Medicare will cover up to 90 days in a benefit period. If you require additional inpatient rehabilitation services, Medicare will cover up to 60 additional days, but you will be responsible for a daily coinsurance payment.
Benefits of Medicare Coverage for Rehabilitation
The benefits of Medicare coverage for rehabilitation are many. For one, rehabilitation services can help you recover from injuries or illnesses faster and more fully. They can also help you maintain your independence and improve your quality of life.
In addition, Medicare coverage for rehabilitation can help you save money on healthcare costs. Without this coverage, you may need to pay for rehabilitation services out of pocket, which can be expensive.
Rehabilitation Coverage Vs. Other Coverage Options
If you have other health insurance coverage, such as a Medicare Advantage plan or private insurance, you may wonder how this coverage compares to Medicare coverage for rehabilitation.
While other insurance plans may offer similar coverage for rehabilitation services, they may have different limits and requirements. It is important to review your plan’s coverage details to understand what services are covered and for how long.
How to Access Medicare Coverage for Rehabilitation
To access Medicare coverage for rehabilitation services, you will need to first be enrolled in Medicare. You can enroll in Medicare by contacting the Social Security Administration or by visiting their website.
Once you are enrolled in Medicare, you can work with your healthcare provider to create a plan of care that includes rehabilitation services. Your provider can then submit this plan to Medicare for approval.
Additional Resources for Medicare Coverage for Rehabilitation
If you have additional questions about Medicare coverage for rehabilitation, there are many resources available to you. You can visit the Medicare website to learn more about rehabilitation services and coverage details.
You can also contact your local Area Agency on Aging, which can provide you with information about local resources for rehabilitation services. Additionally, many healthcare providers and insurance agents can help you navigate the Medicare system and understand your coverage options.
Conclusion
Medicare coverage for rehabilitation services is an important benefit for seniors who need these services. While there are limits to how much coverage you can receive, this coverage can help you recover from injuries or illnesses and improve your quality of life.
If you have questions about Medicare coverage for rehabilitation, be sure to explore the resources available to you and work with your healthcare provider to create a plan of care that meets your needs.
Contents
- Frequently Asked Questions
- How long does Medicare cover rehabilitation?
- What types of rehabilitation services does Medicare cover?
- What is the process for getting rehabilitation services covered by Medicare?
- What happens if I need rehabilitation services for longer than Medicare covers?
- Can I appeal a decision by Medicare to deny coverage for rehabilitation services?
- Medicare Benefits for Rehabilitation in a Skilled Nursing Facility
Frequently Asked Questions
Medicare is a federal health insurance program that covers people who are 65 or older, as well as those with certain disabilities and illnesses. Medicare covers a wide range of medical services, including rehabilitation. If you or a loved one needs rehabilitation, you may have questions about how long Medicare will pay for it. Here are some frequently asked questions and answers about Medicare coverage for rehabilitation.
How long does Medicare cover rehabilitation?
Medicare will cover rehabilitation for as long as it is medically necessary. This means that if your doctor determines that you need rehabilitation to improve your condition or to prevent further deterioration, Medicare will cover the cost. However, Medicare will only cover rehabilitation that is provided by a Medicare-certified provider, and the provider must follow Medicare guidelines for the type and amount of care that is provided.
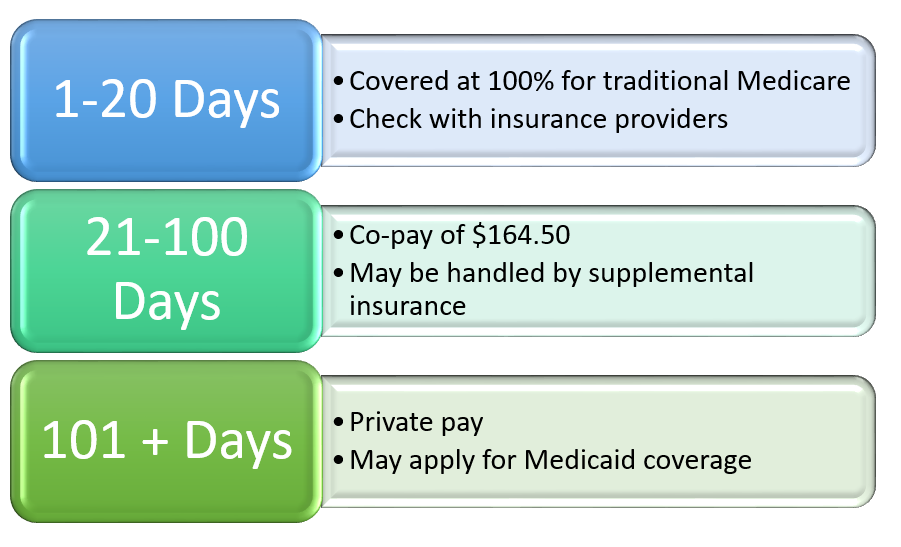
In general, Medicare covers up to 100 days of rehabilitation in a skilled nursing facility or inpatient rehabilitation facility. After the first 20 days, you will need to pay a daily coinsurance amount. If you need rehabilitation services outside of a facility, such as physical therapy or occupational therapy, Medicare will cover the cost as long as it is medically necessary and provided by a Medicare-certified provider.
What types of rehabilitation services does Medicare cover?
Medicare covers a wide range of rehabilitation services, including physical therapy, occupational therapy, and speech-language pathology services. It also covers rehabilitation services provided in a skilled nursing facility or inpatient rehabilitation facility, such as nursing care, room and board, and other services that are necessary for your treatment and recovery. If you need rehabilitation services outside of a facility, such as home health services, Medicare will cover the cost as long as it is medically necessary and provided by a Medicare-certified provider.
It is important to note that Medicare has specific guidelines for the type and amount of rehabilitation services that are covered. Your doctor and rehabilitation provider will work with you to determine the appropriate treatment plan and to ensure that the services you receive are covered by Medicare.
What is the process for getting rehabilitation services covered by Medicare?
If you need rehabilitation services, your doctor will need to provide a referral or order for the services. The rehabilitation provider will then need to submit a plan of care to Medicare, outlining the type and amount of services that are needed. Medicare will review the plan of care and determine whether the services are medically necessary and covered by Medicare.
Once the plan of care is approved, you can begin receiving rehabilitation services. It is important to note that Medicare may only cover a certain amount of services, and you may need to pay a coinsurance or deductible amount. Your rehabilitation provider can help you understand the costs associated with your care and work with you to develop a payment plan if necessary.
What happens if I need rehabilitation services for longer than Medicare covers?
If you need rehabilitation services for longer than Medicare covers, you may need to pay for the services out of pocket, or you may need to explore other options for coverage. Some private insurance plans may cover rehabilitation services, and some states have Medicaid programs that may provide coverage. Your rehabilitation provider can help you understand your options and work with you to develop a plan for continued care.
It is important to remember that Medicare will only cover rehabilitation services that are medically necessary, and your doctor and rehabilitation provider will work with you to determine the appropriate length of treatment based on your condition and progress.
Can I appeal a decision by Medicare to deny coverage for rehabilitation services?
Yes, you have the right to appeal any decision by Medicare to deny coverage for rehabilitation services. If you believe that Medicare has made an incorrect decision, you can file an appeal with Medicare. The appeals process can be complex, but your rehabilitation provider can help you understand the process and provide guidance and support throughout the appeals process.
It is important to remember that you have the right to receive the care that you need, and if you believe that Medicare has denied coverage for necessary rehabilitation services, you should explore your options for appeal and advocacy.
Medicare Benefits for Rehabilitation in a Skilled Nursing Facility
In conclusion, Medicare covers rehabilitation services for a limited period of time. The duration of coverage depends on the patient’s medical condition and progress. It is important to understand that Medicare may not cover all rehabilitation services, and patients may be responsible for some out-of-pocket expenses.
To ensure that you receive the maximum coverage for your rehabilitation needs, it is important to discuss your options with your healthcare provider and Medicare representative. Together, you can create a treatment plan that meets your specific needs and budget.
In the end, Medicare provides a valuable service to those in need of rehabilitation services. By understanding the coverage options available, patients can make informed decisions about their care and focus on their recovery without the added stress of financial burden.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts