Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
Medicare is a government-sponsored health insurance program that helps millions of Americans afford medical care. Unfortunately, some individuals and organizations take advantage of the system by committing fraud and abuse. Medicare fraud and abuse can have serious consequences, both for the individuals involved and for the integrity of the program as a whole.
Medicare fraud occurs when someone intentionally submits false claims or information in order to receive payments from the program. Medicare abuse, on the other hand, refers to practices that are inconsistent with accepted medical standards and result in unnecessary costs to the program. In this article, we will explore what constitutes Medicare fraud and abuse, the impact it has on the program, and what steps are being taken to prevent it.
Contents
- Understanding Medicare Fraud and Abuse
- What is Medicare Fraud?
- What is Medicare Abuse?
- The Impact of Medicare Fraud and Abuse
- Examples of Medicare Fraud and Abuse
- Preventing Medicare Fraud and Abuse
- The Benefits of Preventing Medicare Fraud and Abuse
- Medicare Fraud and Abuse vs. Waste
- The Role of the Government in Preventing Medicare Fraud and Abuse
- In Conclusion
- Frequently Asked Questions
Understanding Medicare Fraud and Abuse
Medicare is a government-funded health insurance program that provides coverage to millions of Americans, including those who are 65 years and older, those with certain disabilities, and those with end-stage renal disease. Unfortunately, some individuals and organizations take advantage of the Medicare system by committing fraud and abuse. This can result in significant financial losses for the government and can even put patients at risk.
What is Medicare Fraud?
Medicare fraud involves intentionally billing Medicare for services, procedures, or supplies that were never provided or were unnecessary. This can include submitting false claims, forging or altering medical records, and offering or receiving kickbacks for referrals. Medicare fraud can be committed by healthcare providers, patients, or even individuals who work for Medicare.
To combat Medicare fraud, the government has implemented several measures, including increased oversight, education, and enforcement. Patients can also help prevent Medicare fraud by reviewing their Medicare summary notices and reporting any suspicious activity.
What is Medicare Abuse?
Medicare abuse involves practices that are inconsistent with accepted medical, business, or fiscal practices. This can include billing for services that are not medically necessary, providing unnecessary or excessive services, or charging Medicare more than the actual cost of a service or supply. Unlike fraud, Medicare abuse may not be intentional, but it still results in unnecessary costs for the program.
To prevent Medicare abuse, healthcare providers must ensure that they are following appropriate medical and billing practices. They should review Medicare guidelines regularly and seek guidance from Medicare if they are unsure about a particular service or practice.
The Impact of Medicare Fraud and Abuse
Medicare fraud and abuse can have significant consequences for patients, healthcare providers, and the government. Patients may receive unnecessary or harmful treatments, and their personal information may be compromised. Healthcare providers may face legal and financial consequences, and their reputations may be damaged. The government may lose billions of dollars each year due to fraudulent and abusive practices, which can ultimately impact the availability and quality of healthcare services.
Examples of Medicare Fraud and Abuse
There are several types of Medicare fraud and abuse that are commonly reported, including:
- Submitting false claims for services or supplies that were never provided
- Charging Medicare for unnecessary or excessive services
- Falsifying medical records or billing codes
- Offering or receiving kickbacks for referrals
- Using unlicensed or untrained staff to provide services
These practices can occur in various healthcare settings, such as hospitals, nursing homes, and home health agencies.
Preventing Medicare Fraud and Abuse
Preventing Medicare fraud and abuse requires a collaborative effort between patients, healthcare providers, and the government. Patients can help prevent fraud and abuse by reviewing their Medicare summary notices and reporting any suspicious activity. Healthcare providers must follow appropriate medical and billing practices and seek guidance from Medicare if they are unsure about a particular service or practice. The government has implemented several measures to combat fraud and abuse, including increased oversight and enforcement.
The Benefits of Preventing Medicare Fraud and Abuse
Preventing Medicare fraud and abuse can have several benefits, including:
- Reducing healthcare costs for patients and the government
- Improving the quality of healthcare services
- Protecting patient privacy and personal information
- Ensuring that healthcare providers are following appropriate medical and billing practices
By preventing fraud and abuse, patients can receive the care they need without unnecessary costs or risks, and healthcare providers can maintain their reputations and avoid legal and financial consequences.
Medicare Fraud and Abuse vs. Waste
It is important to distinguish between Medicare fraud and abuse and Medicare waste. Medicare waste involves inefficient or unnecessary practices that result in unnecessary costs for the program, but do not involve intentional or abusive practices. While Medicare waste should still be addressed and reduced, it is not as serious as fraud and abuse, which can have significant financial and legal consequences.
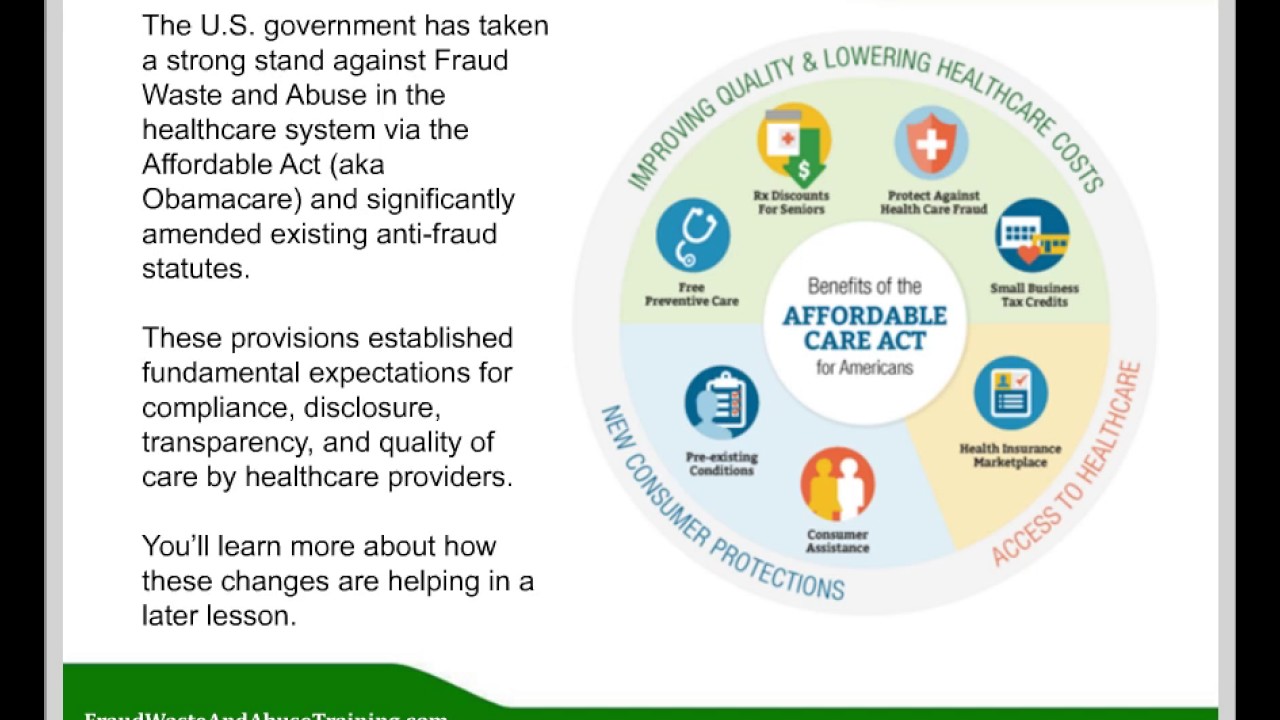
The Role of the Government in Preventing Medicare Fraud and Abuse
The government plays a critical role in preventing Medicare fraud and abuse. The Centers for Medicare and Medicaid Services (CMS) has implemented several measures to combat fraud and abuse, including:
- Increased oversight and enforcement
- Education and awareness programs for healthcare providers and patients
- Collaboration with law enforcement agencies to investigate and prosecute fraudulent activity
- Implementation of new technologies and systems to detect and prevent fraud and abuse
By taking these measures, the government can help protect the integrity of the Medicare program and ensure that patients receive the care they need without unnecessary costs or risks.
In Conclusion
Medicare fraud and abuse are serious problems that can have significant consequences for patients, healthcare providers, and the government. By understanding what Medicare fraud and abuse are, how they can be prevented, and the role of the government in combating these practices, patients and healthcare providers can work together to ensure that Medicare is used appropriately and efficiently.
Frequently Asked Questions
Medicare fraud and abuse are serious issues that can lead to financial losses for both the government and beneficiaries. Here are some common questions and answers about Medicare fraud and abuse:
What is Medicare fraud?
Medicare fraud occurs when healthcare providers or suppliers intentionally bill Medicare for services or supplies that were not provided, were unnecessary, or were more expensive than what was actually provided. This can include submitting false claims, kickbacks, and accepting bribes in exchange for services or supplies. Medicare fraud can result in significant financial losses for Medicare and can also harm beneficiaries by providing them with unnecessary or harmful services.
Examples of Medicare fraud include billing for services not rendered, billing for more expensive services than what was provided, and upcoding (billing for a more expensive service than what was actually provided). Medicare fraud can also involve identity theft, where someone uses another person’s Medicare information to obtain services or supplies.
What is Medicare abuse?
Medicare abuse is not the same as fraud, but it can still lead to financial losses for Medicare and harm beneficiaries. Medicare abuse occurs when healthcare providers or suppliers provide services or supplies that are not medically necessary or that do not meet professional standards of care. Medicare abuse can include overusing services or supplies, providing unnecessary services or supplies, and billing for services or supplies that are not covered by Medicare.
Examples of Medicare abuse include performing unnecessary tests or procedures, prescribing unnecessary medications, and charging excessive fees for services or supplies. Medicare abuse can also involve improper coding of services, which can result in overpayment from Medicare.
What are the consequences of Medicare fraud and abuse?
Medicare fraud and abuse can result in significant financial losses for Medicare, which can lead to higher costs and reduced benefits for beneficiaries. Additionally, Medicare fraud and abuse can harm beneficiaries by providing them with unnecessary or harmful services or supplies. Healthcare providers and suppliers who engage in Medicare fraud and abuse can face criminal and civil penalties, including fines, imprisonment, and exclusion from Medicare.
Beneficiaries who suspect Medicare fraud or abuse can report it to the Medicare program, which can investigate and take action against healthcare providers and suppliers who engage in fraudulent or abusive practices.
How can I protect myself from Medicare fraud and abuse?
There are several steps you can take to protect yourself from Medicare fraud and abuse. These include reviewing your Medicare Summary Notice (MSN) or Explanation of Benefits (EOB) statements to ensure that you received the services or supplies listed and that they were necessary. You should also keep track of your Medicare card and only give your Medicare information to trusted healthcare providers or suppliers.
If you have any questions or concerns about Medicare fraud or abuse, you can contact your local Senior Medicare Patrol (SMP) program, which provides free education and assistance to Medicare beneficiaries on how to prevent, detect, and report fraud and abuse.
What should I do if I suspect Medicare fraud or abuse?
If you suspect Medicare fraud or abuse, you should report it to the Medicare program as soon as possible. You can call the Medicare hotline at 1-800-MEDICARE (1-800-633-4227) or contact your local SMP program for assistance. You should also keep any documentation related to the suspected fraud or abuse, such as billing statements or receipts.
The Medicare program takes reports of fraud and abuse seriously and will investigate and take action against healthcare providers and suppliers who engage in fraudulent or abusive practices.
How Medicare And Medicaid Fraud Became A $100B Problem In The U.S.
In conclusion, Medicare fraud and abuse are serious issues that can have far-reaching consequences for both individuals and the healthcare system as a whole. It is essential to understand what they are, how they can occur, and how to prevent them from happening. By being vigilant and reporting any suspicious activity, we can help ensure that Medicare resources are used appropriately and that those who need them the most receive the care they deserve.
Furthermore, it is important to remember that Medicare fraud and abuse can take many forms, including billing for services that were never provided, providing unnecessary services or equipment, and using kickbacks to receive payments for referrals. These actions not only harm patients by providing substandard care, but they also cost taxpayers billions of dollars each year.
Ultimately, preventing Medicare fraud and abuse requires a collaborative effort between healthcare providers, patients, and government agencies. By working together, we can help ensure that Medicare resources are used effectively and efficiently, and that those who seek to take advantage of the system are held accountable for their actions.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts