Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
Medicare is a federal health insurance program that covers millions of Americans aged 65 and older. It also covers people with certain disabilities and those with end-stage renal disease. As people age, they may require rehabilitation services to regain their strength, mobility, and independence. But how long will Medicare pay for rehab? This is a critical question that many Medicare beneficiaries and their families ask, and the answer depends on several factors.
In this article, we will explore the different types of rehab services that Medicare covers, the duration of coverage, and the conditions that must be met for continued eligibility. We will also discuss some of the limitations and costs associated with Medicare rehab coverage. If you or a loved one needs rehab services, this article will provide you with valuable information to help you navigate the Medicare system and make informed decisions about your healthcare.
Medicare provides coverage for up to 100 days of rehabilitation care in a skilled nursing facility per benefit period. However, there are certain requirements that must be met to qualify for this coverage, including a prior hospital stay of at least three days and a physician’s order for skilled nursing care. After the initial coverage period, Medicare may still cover some of the costs, but it will be at a reduced rate. It is important to check with your healthcare provider and Medicare to determine your specific coverage and costs.
How Long Will Medicare Pay for Rehab?
Rehabilitation services are an important aspect of medical care, particularly for seniors. As we age, it’s common to experience injuries or illnesses that require specialized care in order to regain our strength and independence. Medicare is a health insurance program that provides coverage for a wide range of medical services, including rehabilitation. But how long will Medicare pay for rehab? Let’s take a closer look.
Medicare Coverage for Rehabilitation Services
Medicare Part A and Part B both provide coverage for rehabilitation services. Part A covers inpatient rehabilitation services, while Part B covers outpatient rehabilitation services. Both types of coverage have their own specific rules and limitations.
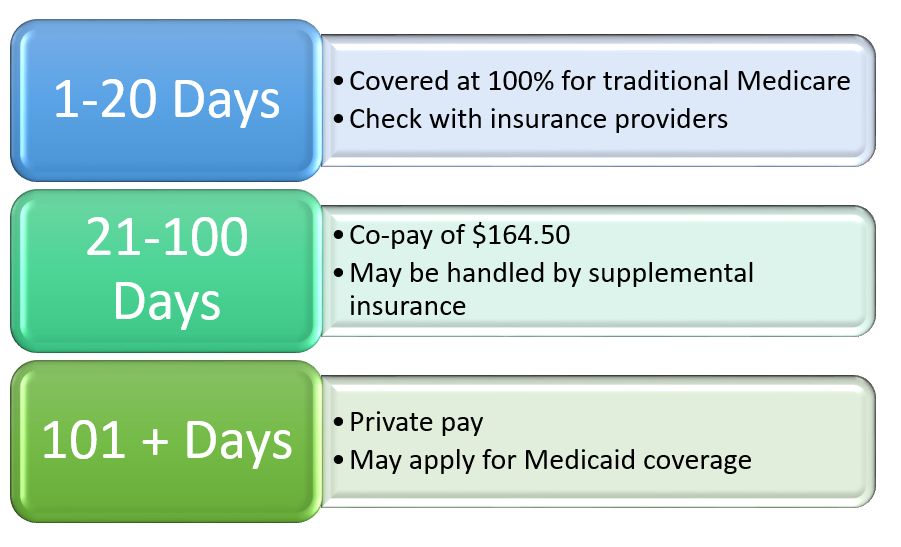
For inpatient rehabilitation services, Medicare Part A will cover up to 100 days of care in a skilled nursing facility or inpatient rehabilitation facility. However, there are certain requirements that must be met in order to qualify for this coverage. The patient must have been admitted to the hospital for at least three consecutive days and require daily skilled nursing or rehabilitation services in order to qualify for Part A coverage.
For outpatient rehabilitation services, Medicare Part B will cover a wide range of services, including physical therapy, occupational therapy, and speech therapy. There are no limits on the number of outpatient rehabilitation services that Medicare Part B will cover, as long as the services are deemed medically necessary and provided by a Medicare-approved provider.
Additional Medicare Coverage for Rehabilitation Services
In addition to the coverage provided by Medicare Part A and Part B, there are other Medicare programs that may provide coverage for rehabilitation services. For example, Medicare Advantage plans, also known as Medicare Part C, often provide additional benefits beyond what is covered by traditional Medicare. Some Medicare Advantage plans may include coverage for in-home rehabilitation services or extended coverage for outpatient rehabilitation services.
Another program that may provide additional coverage for rehabilitation services is Medicare Supplement Insurance, also known as Medigap. Medigap policies are designed to fill in the gaps in coverage left by traditional Medicare, and may provide coverage for co-payments, deductibles, and other out-of-pocket costs associated with rehabilitation services.
Benefits of Medicare Coverage for Rehabilitation Services
The benefits of Medicare coverage for rehabilitation services are clear. Rehabilitation services are an essential part of the recovery process for many seniors, and can help them regain their independence and quality of life. By providing coverage for these services, Medicare helps ensure that seniors have access to the care they need to stay healthy and active.
In addition to the physical benefits of rehabilitation services, there are also financial benefits to Medicare coverage. Rehabilitation services can be expensive, particularly if they are needed for an extended period of time. By providing coverage for these services, Medicare helps protect seniors from the financial burden of paying for these services out of pocket.
Conclusion
In conclusion, Medicare provides coverage for a wide range of rehabilitation services, including both inpatient and outpatient services. While there are limitations on the amount of coverage provided by Medicare Part A, there are no limits on the number of outpatient rehabilitation services covered by Medicare Part B. In addition to the coverage provided by traditional Medicare, there are also other programs, such as Medicare Advantage and Medigap, that may provide additional coverage for rehabilitation services. By providing coverage for these services, Medicare helps ensure that seniors have access to the care they need to stay healthy and independent.
Contents
Frequently Asked Questions
1. How long will Medicare pay for rehab?
Medicare will pay for a certain amount of rehab days, depending on the type of rehab you need. If you need inpatient rehab, Medicare will cover up to 100 days in a benefit period. If you need outpatient rehab, Medicare will cover as many sessions as deemed necessary by your healthcare provider.
It is important to note that Medicare will only cover rehab services that are deemed medically necessary and provided by a Medicare-approved facility or healthcare provider. Once you have reached your coverage limit, you will be responsible for any additional costs.
2. What types of rehab does Medicare cover?
Medicare will cover a variety of rehab services, including physical therapy, occupational therapy, and speech therapy. Inpatient rehab facilities may also offer other services such as nursing care, meals, and social activities. Outpatient rehab may include services such as individual therapy, group therapy, and specialized programs for specific conditions.
It is important to check with your healthcare provider or Medicare to ensure that the rehab services you need are covered and to get a full understanding of your coverage limits.
3. Do I need a referral to receive rehab services?
In most cases, you will need a referral from your healthcare provider to receive rehab services. This will ensure that the rehab services you receive are medically necessary and appropriate for your condition. Your healthcare provider will work with you to determine the best course of treatment and may refer you to a specific rehab facility or provider.
If you are enrolled in a Medicare Advantage plan, you may need to follow specific guidelines and obtain prior authorization before receiving rehab services.
4. Can I receive rehab services at home?
Yes, Medicare will cover certain home health services, including rehab services if deemed medically necessary. Your healthcare provider will determine if you meet the criteria for home health services and will work with you to develop a plan of care.
Home health services may include physical therapy, occupational therapy, speech therapy, and other services. It is important to note that Medicare will only cover home health services that are provided by a Medicare-approved home health agency.
5. What happens if I exceed my coverage limit for rehab services?
If you exceed your coverage limit for rehab services, you will be responsible for any additional costs. You may also choose to pay out of pocket for additional rehab services if you feel they are necessary for your recovery.
It is important to work with your healthcare provider and Medicare to ensure that you are receiving the appropriate level of care and that you understand your coverage limits. Your healthcare provider may also be able to recommend other resources or programs that can help you with your recovery.
Will Medicare pay for rehab?
In conclusion, the duration of Medicare coverage for rehab services depends on the individual’s condition and the type of care needed. While some individuals may receive coverage for up to 100 days, others may not qualify for Medicare coverage at all. It is important to speak with a healthcare provider and the Medicare program to determine what coverage options are available and what services are covered.
Additionally, it is important to note that Medicare coverage for rehab services may be subject to limitations and restrictions. For example, some rehab services may only be covered if they are deemed medically necessary and if they are provided by an approved healthcare provider. It is important to understand these limitations and restrictions to ensure that you receive the appropriate coverage and care.
Overall, if you or a loved one requires rehab services, it is important to explore all coverage options and to work with healthcare providers to determine the best course of action. With the right care and support, individuals can receive the rehabilitation services they need to improve their health and wellbeing.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts