Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
As healthcare providers, it is essential to understand the eligibility requirements for Medicare. With the increasing number of seniors in the United States, Medicare is becoming an important part of the healthcare system. However, checking Medicare eligibility for providers can be a daunting task, especially for those who are new to the industry.
In this article, we will discuss how to check Medicare eligibility for providers in a straightforward and concise manner. We will cover the basics of Medicare, the eligibility requirements for providers, and the steps you need to take to verify Medicare status. Whether you are a healthcare provider, a billing specialist, or simply looking to learn more about Medicare, this article will provide you with the information you need to ensure you are providing the best care possible.
To check Medicare eligibility for providers, follow the steps below:
- Visit the Medicare Provider Eligibility and Enrollment Lookup tool on the CMS website.
- Enter the provider’s National Provider Identifier (NPI) or the Provider Transaction Access Number (PTAN).
- Verify the provider’s information and eligibility status.
Contents
- How to Check Medicare Eligibility for Providers?
- Frequently Asked Questions
- What is Medicare eligibility for providers?
- How can providers check their Medicare eligibility status?
- What are the requirements for Medicare provider eligibility?
- What is the Medicare Provider Enrollment, Chain, and Ownership System (PECOS)?
- What should providers do if they are not eligible for Medicare?
- Medicare Eligibility Verification | Medicare Eligibility Check – Episode Alert
How to Check Medicare Eligibility for Providers?
As a healthcare provider, it is essential to know whether your patients are eligible for Medicare coverage. Medicare is a federal health insurance program that provides coverage for individuals who are 65 years or older, have certain disabilities, or have End-Stage Renal Disease (ESRD). In this article, we will discuss how to check Medicare eligibility for providers.
Understanding Medicare Eligibility Requirements
To check Medicare eligibility for your patients, it is important to understand the eligibility requirements. Medicare is divided into four parts: Part A, Part B, Part C, and Part D. Here are the eligibility requirements for each part:
Part A: Individuals who are 65 years or older, have received Social Security benefits for at least 24 months, or have ESRD or amyotrophic lateral sclerosis (ALS) are eligible for Part A.
Part B: Individuals who are 65 years or older, have ESRD, ALS, or have been receiving disability benefits for at least 24 months are eligible for Part B.
Part C: Individuals who are eligible for Part A and Part B are also eligible for Part C, also known as Medicare Advantage.
Part D: Individuals who are eligible for Part A and/or Part B are also eligible for Part D, which provides prescription drug coverage.
Once you understand the eligibility requirements, you can check your patient’s Medicare eligibility.
Ways to Check Medicare Eligibility
There are several ways to check Medicare eligibility for your patients:
1. Medicare Administrative Contractor (MAC) Portal: Medicare Administrative Contractors (MACs) are responsible for processing Medicare claims. You can check your patient’s eligibility by logging into the MAC portal using your National Provider Identifier (NPI) number.
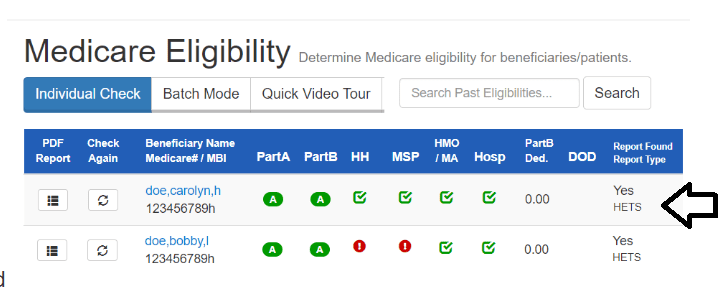
2. Medicare Beneficiary Eligibility (MBE) Transaction: MBE is a transaction that allows you to check your patient’s eligibility and benefits. You can use this transaction through your clearinghouse or billing service.
3. Interactive Voice Response (IVR) System: You can use the IVR system to check your patient’s eligibility by calling the Medicare provider helpline.
4. Online Eligibility Checker: There are several online eligibility checkers that allow you to check your patient’s eligibility by entering their information.
Once you have checked your patient’s eligibility, you can determine whether their Medicare coverage is active and what services are covered under their plan.
Benefits of Checking Medicare Eligibility
Checking your patient’s Medicare eligibility has several benefits. It allows you to determine whether your patient’s Medicare coverage is active and what services are covered under their plan. This helps you provide the appropriate care for your patient and ensures that you receive timely reimbursement for your services.
Conclusion
In conclusion, checking Medicare eligibility for providers is essential to ensure that your patients receive the appropriate care and that you receive timely reimbursement for your services. By understanding the eligibility requirements and using the available resources, you can easily check your patient’s Medicare eligibility and provide the best care possible.
Frequently Asked Questions
Read below for answers to common questions about how to check Medicare eligibility for providers.
What is Medicare eligibility for providers?
Medicare eligibility for providers refers to the ability of a healthcare provider or facility to accept Medicare insurance for payment of medical services. Providers must meet certain qualifications and enroll with Medicare to be eligible to receive payment from the program.
As a healthcare provider, it is important to understand Medicare eligibility requirements and ensure that your practice is enrolled with Medicare to ensure timely payment and compliance with regulations.
How can providers check their Medicare eligibility status?
Providers can check their Medicare eligibility status by logging into the Medicare Provider Enrollment, Chain, and Ownership System (PECOS) and reviewing their enrollment information. Providers can also contact their Medicare Administrative Contractor (MAC) for assistance with checking their eligibility status.
It is important for providers to regularly review their Medicare enrollment status to ensure that their information is up-to-date and accurate. Any changes to a provider’s enrollment information should be reported to Medicare as soon as possible.
What are the requirements for Medicare provider eligibility?
The requirements for Medicare provider eligibility vary depending on the type of provider or facility. Generally, providers must be licensed and accredited in their state, meet certain quality standards, and comply with Medicare billing and coding requirements.
Providers must also enroll with Medicare and maintain their enrollment status to be eligible to receive payment from the program. Providers who do not meet these requirements may be subject to penalties or exclusion from the Medicare program.
What is the Medicare Provider Enrollment, Chain, and Ownership System (PECOS)?
The Medicare Provider Enrollment, Chain, and Ownership System (PECOS) is an online portal for providers to enroll and manage their Medicare enrollment information. Providers can use PECOS to update their information, check their enrollment status, and submit claims for payment.
PECOS is an important tool for providers to ensure that their Medicare enrollment information is up-to-date and accurate. Providers should regularly review their information in PECOS and make any necessary updates to avoid delays in payment or compliance issues.
What should providers do if they are not eligible for Medicare?
If a provider is not eligible for Medicare, they may need to explore other insurance options or payment arrangements with patients. Providers may also consider enrolling in other government programs, such as Medicaid or private insurance plans, to expand their patient base and increase revenue.
It is important for providers to understand their insurance options and eligibility requirements to ensure that they are able to provide high-quality care to their patients and maintain a sustainable practice.
Medicare Eligibility Verification | Medicare Eligibility Check – Episode Alert
In conclusion, checking Medicare eligibility for providers can be a daunting task, but it is crucial to ensure that you are able to provide quality care to your patients while also receiving proper reimbursement. By understanding the requirements and guidelines set forth by Medicare, you can easily determine your eligibility and avoid any potential penalties or fines.
Moreover, it is important to stay up-to-date with any changes or updates to Medicare eligibility criteria to ensure that you are always in compliance. This can be achieved by regularly checking the Medicare website or consulting with a healthcare attorney or consultant.
Ultimately, taking the time to check Medicare eligibility for providers is a necessary step in maintaining a successful healthcare practice. By doing so, you can ensure that you are providing the best possible care to your patients while also protecting your practice from any legal or financial repercussions.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts