Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
Are you struggling to navigate the complex process of filing an appeal with Medicare? You’re not alone. With so many rules and regulations, it can be overwhelming to know where to start. However, it’s important to understand your rights as a Medicare beneficiary and to know how to file an appeal if you believe you’ve been denied coverage unfairly. In this guide, we’ll break down the steps you need to take to file an appeal with Medicare and get the coverage you need. So let’s get started!
How to File an Appeal With Medicare
Medicare is a federal health insurance program that provides coverage for people aged 65 and older, as well as those with certain disabilities. While Medicare covers many medical services, there may be instances when a claim is denied or a service is not covered. If this happens, you have the right to file an appeal with Medicare to try and get the decision reversed. Here’s what you need to know about filing an appeal with Medicare.
Understanding Medicare Appeals
When you receive medical care that is covered under Medicare, the healthcare provider sends a bill to Medicare for payment. If Medicare denies the claim or doesn’t cover a service, you will receive a notice explaining the decision. This notice will also explain your right to appeal the decision.
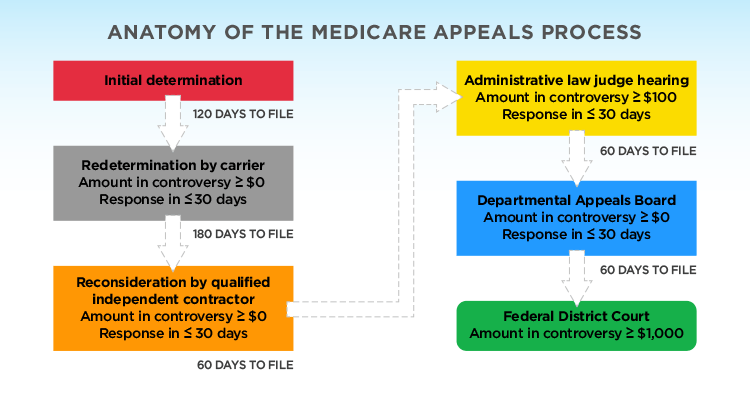
There are five levels of appeals that you can go through if you want to challenge a Medicare decision. The first level is a redetermination, followed by a reconsideration, a hearing by an administrative law judge, a review by the Medicare Appeals Council, and finally, a review by a federal court.
Steps to Filing an Appeal
If you want to file an appeal with Medicare, you will need to follow these steps:
Step 1: Review Your Medicare Summary Notice
This notice will explain the reason for the denial or non-coverage of the service. It will also provide instructions on how to file an appeal.
Step 2: Fill Out a Redetermination Request Form
This form can be found on the back of your Medicare Summary Notice. Make sure to fill it out completely and provide any additional information or documentation that may support your appeal.
Step 3: Submit Your Request
You can submit your request online, by mail, or by fax. Make sure to keep a copy of your request for your records.
Step 4: Wait for a Response
You should receive a response within 60 days of submitting your request. If your redetermination request is denied, you can move on to the next level of appeal.
Additional Information
Here are some important things to keep in mind when filing an appeal with Medicare:
Benefit of Filing an Appeal
Filing an appeal with Medicare can be beneficial because it gives you the opportunity to challenge a decision that you believe is incorrect. This can result in the coverage of a service that was previously denied or non-covered.
Time Limits
There are time limits for filing an appeal with Medicare. Make sure to file your appeal within the specified time frame to avoid missing out on your opportunity to challenge the decision.
Representation
You have the right to be represented by an attorney or other qualified representative when filing an appeal with Medicare. This can be especially helpful if you are unsure about the appeals process or need assistance in preparing your appeal.
Costs
There are no costs associated with filing an appeal with Medicare. However, if you choose to be represented by an attorney or other representative, there may be fees associated with their services.
Appealing a Medicare Advantage Plan Decision
If you are enrolled in a Medicare Advantage plan, you will need to follow the appeals process outlined by your plan. This may differ from the appeals process for original Medicare.
Conclusion
Filing an appeal with Medicare can be a complex process, but it is important to understand your rights and options if you believe a decision is incorrect. Follow the steps outlined above and seek representation if necessary to ensure the best possible outcome for your appeal. Remember to file your appeal within the specified time frame and keep copies of all documentation for your records.
Frequently Asked Questions
If you disagree with a coverage decision made by Medicare, you have the right to file an appeal. Here are some common questions about how to file an appeal.
1. What is an appeal, and when can I file one?
An appeal is a formal request to review a decision made by Medicare about your health care coverage. You can file an appeal if Medicare has denied coverage for a medical service or treatment you believe is necessary. You can also file an appeal if you disagree with the amount you have been asked to pay for a service or treatment that Medicare has covered.
It’s important to note that you can only file an appeal if you have received a Medicare Summary Notice (MSN) or a denial letter from Medicare. You must file your appeal within 120 days from the date on the MSN or denial letter.
2. How do I file an appeal?
The first step in filing an appeal is to review the MSN or denial letter you received from Medicare. This will provide information about why the service or treatment was denied and how to file an appeal. You can also call the phone number on your MSN or denial letter to get more information about the appeals process.
To file an appeal, you will need to complete a “Redetermination Request Form” and send it to the address listed on your MSN or denial letter. You can also submit your appeal online through the Medicare website. Be sure to include any additional documentation or medical records that support your appeal.
3. What happens after I file an appeal?
After you file your appeal, Medicare will review your case and make a decision. If Medicare denies your appeal, you have the right to request a hearing with an administrative law judge. If the judge also denies your appeal, you can appeal to the Medicare Appeals Council. If your appeal is still denied, you can file a lawsuit in federal court.
It’s important to note that the appeals process can be lengthy, so be prepared to wait several months for a decision. You can also request an expedited appeal if you believe the standard appeals process would cause serious harm to your health.
4. Can I get help filing an appeal?
Yes, there are several resources available to help you file an appeal. You can contact your State Health Insurance Assistance Program (SHIP) for free assistance with the appeals process. You can also contact your local Medicare office or the Medicare Beneficiary Ombudsman for help.
If you have a Medicare Advantage or Part D plan, you can also contact your plan directly for assistance with filing an appeal.
5. What are my rights if my appeal is successful?
If your appeal is successful, Medicare will provide coverage for the service or treatment that was previously denied. You will also receive a refund for any out-of-pocket costs you paid for the service or treatment. If you paid for the service or treatment out-of-pocket and did not receive reimbursement, you can also file a claim for reimbursement.
Keep in mind that if you have a Medicare Advantage plan, your plan may have different rules about coverage and appeals. Be sure to review your plan’s coverage documents and contact your plan for more information.
How can I appeal a denial of Medicare coverage?
In conclusion, filing an appeal with Medicare might seem like a daunting task, but it is important to remember that you have the right to appeal any decision made by Medicare. By following the proper steps, you can ensure your voice is heard and you receive the coverage you deserve.
Remember to carefully review your Medicare Summary Notice and any denial letters you receive before filing an appeal. Keep track of all important dates and deadlines, and consider seeking assistance from a qualified professional if needed.
Most importantly, don’t give up. Your health and well-being are worth fighting for, and with the right approach, you can successfully file an appeal with Medicare and receive the care you need.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts