Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify...Read more
Medicare is a government-funded health insurance program that provides coverage for a wide range of medical services and supplies. However, many people are left wondering if Medicare covers crutches, which can be essential for those with mobility issues.
If you or a loved one is in need of crutches, it’s important to understand your coverage options under Medicare. In this article, we’ll explore the ins and outs of Medicare coverage for crutches and provide you with the information you need to make informed decisions about your healthcare. So, let’s dive in!
Yes, Medicare Part B covers crutches when they are medically necessary to aid in mobility or recovery from an injury or surgery. Medicare will cover 80% of the cost of crutches, and the remaining 20% will be the responsibility of the patient. In most cases, Medicare will require a doctor’s prescription for crutches. It is important to check with your specific Medicare plan to confirm coverage and any out-of-pocket costs.
Does Medicare Cover Crutches?
If you or a loved one has suffered an injury or undergone surgery, you may be in need of crutches to aid in mobility during the recovery process. The question arises, does Medicare cover the cost of crutches? In short, the answer is yes. However, there are certain guidelines and limitations that must be followed to ensure coverage.
Medicare Part B Coverage
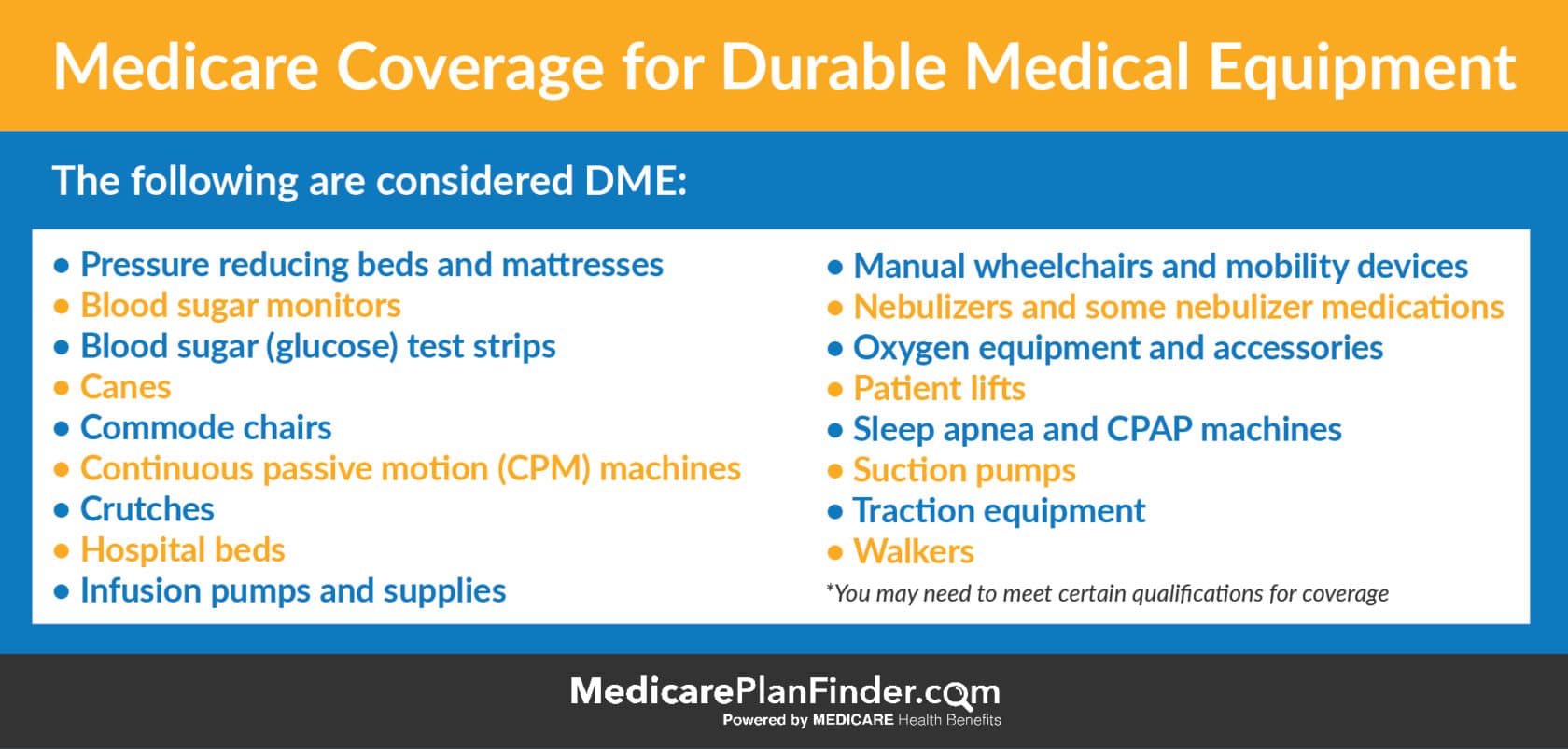
Medicare Part B covers durable medical equipment (DME), including crutches, when they are deemed medically necessary. This means that the crutches must be prescribed by a doctor and used for a specific medical condition or injury. Medicare will cover 80% of the cost, and the remaining 20% will be the responsibility of the patient or their supplemental insurance plan.
It is important to note that Medicare will only cover the cost of crutches that meet their specific guidelines. This includes crutches that are adjustable, made of sturdy material, and have non-slip tips to prevent falls. Crutches that are not deemed medically necessary, such as those used for temporary convenience, will not be covered.
How to Obtain Coverage
To obtain coverage for crutches under Medicare Part B, a doctor’s prescription must be obtained. The prescription should include the medical necessity for the crutches and the length of time they will be needed. Once the prescription is obtained, the patient can obtain the crutches through a Medicare-approved DME supplier.
It is important to note that not all DME suppliers are approved by Medicare. Patients should ensure that the supplier they choose is approved by Medicare to avoid any additional out-of-pocket costs.
Benefits of Medicare Coverage
Medicare coverage for crutches can provide significant financial relief for those in need. Rather than paying the full cost out of pocket, Medicare will cover 80% of the cost, with the remaining 20% covered by supplemental insurance or paid by the patient.
In addition to financial benefits, Medicare coverage for crutches ensures that patients have access to quality, medically necessary equipment. This can aid in the recovery process and prevent further injury or complications.
Crutches vs. Other Mobility Aids
While crutches are a common form of mobility aid, they may not be the best option for everyone. Medicare also covers other forms of mobility aids, including canes, walkers, and wheelchairs.
The choice of mobility aid will depend on the specific medical condition or injury, as well as the individual’s mobility needs. It is important to consult with a doctor to determine the best form of mobility aid for each individual case.
Conclusion
In summary, Medicare does cover the cost of crutches when they are deemed medically necessary. Patients must obtain a doctor’s prescription and obtain the crutches through a Medicare-approved DME supplier. Medicare will cover 80% of the cost, with the remaining 20% covered by supplemental insurance or paid by the patient.
It is important to follow Medicare’s guidelines for crutches to ensure coverage. Patients should also consider other forms of mobility aids, depending on their specific medical condition and mobility needs. Overall, Medicare coverage for crutches can provide significant financial relief and aid in the recovery process.
Frequently Asked Questions
Does Medicare Cover Crutches?
Yes, Medicare covers crutches as durable medical equipment (DME) for beneficiaries who need them to move around due to an injury or illness. To be eligible for coverage, the crutches must be prescribed by a doctor, and the supplier must be enrolled in Medicare.
It’s important to note that Medicare only covers the cost of the crutches, not any additional accessories or upgrades. Additionally, if the beneficiary chooses to rent crutches instead of purchasing them, Medicare may only cover a portion of the rental cost.
In summary, Medicare does cover crutches as DME, but certain conditions must be met for coverage to be granted. It’s always best to consult with a doctor and a Medicare representative to ensure proper coverage and reimbursement.
How Do I Get Crutches Covered by Medicare?
To get crutches covered by Medicare, you must first have a doctor’s prescription for the crutches as durable medical equipment (DME). The supplier who provides the crutches must also be enrolled in Medicare and accept assignment.
Once these requirements are met, the supplier will submit a claim to Medicare on your behalf. If the claim is approved, Medicare will cover the cost of the crutches, but you may be responsible for a portion of the cost depending on your specific Medicare plan.
It’s important to keep in mind that Medicare only covers the cost of the crutches themselves, not any additional accessories or upgrades. If you have any questions or concerns about coverage, it’s best to consult with a Medicare representative or your healthcare provider.
Can I Rent Crutches Through Medicare?
Yes, Medicare may cover the cost of renting crutches as durable medical equipment (DME) if the beneficiary meets certain eligibility requirements. The rental period may be for up to 13 months, with the option to purchase the crutches at the end of the rental period if desired.
To be eligible for rental coverage, the crutches must be prescribed by a doctor, and the supplier must be enrolled in Medicare. Additionally, the beneficiary must have a medical need for the crutches and must not have previously received a similar item.
It’s important to note that if the beneficiary chooses to rent crutches instead of purchasing them, Medicare may only cover a portion of the rental cost. It’s always best to consult with a Medicare representative or your healthcare provider to determine the best course of action for your specific situation.
What Types of Crutches Does Medicare Cover?
Medicare covers several types of crutches as durable medical equipment (DME), including underarm crutches, forearm crutches, and platform crutches. The type of crutches prescribed will depend on the beneficiary’s specific medical needs and mobility restrictions.
In addition to standard crutches, Medicare may also cover specialized crutches, such as those with shock-absorbing features or those designed for pediatric patients. However, it’s important to note that Medicare only covers the cost of the crutches themselves, not any additional accessories or upgrades.
If you have any questions or concerns about the types of crutches covered by Medicare, it’s best to consult with your healthcare provider or a Medicare representative.
Are There Any Other Options for Mobility Aids Covered by Medicare?
Yes, Medicare covers several other options for mobility aids besides crutches, including walkers, canes, and power wheelchairs. Like crutches, these items must be prescribed by a doctor and supplied by a Medicare-enrolled supplier.
The specific type of mobility aid prescribed will depend on the beneficiary’s mobility needs and restrictions. Medicare may cover a portion or all of the cost of the mobility aid, depending on the specific plan and coverage.
If you have any questions or concerns about your eligibility for mobility aids covered by Medicare, it’s best to consult with a healthcare provider or a Medicare representative.
Will Medicare Cover My Procedure? What’s Covered by Medicare
In conclusion, Medicare coverage for crutches is available for eligible beneficiaries. However, it is important to note that not all types of crutches are covered, and there may be certain criteria that must be met in order to qualify for coverage. It’s always important to check with your healthcare provider and Medicare to determine your specific coverage options.
Additionally, while Medicare may cover a portion of the cost of crutches, there may still be out-of-pocket expenses that you will need to consider. It’s important to weigh the costs and benefits of different crutch options before making a decision.
Ultimately, if you require crutches for mobility assistance, it’s important to explore your coverage options under Medicare. With the right information and resources, you can make an informed decision about your healthcare needs and ensure that you receive the support you need to maintain your independence and quality of life.
Introducing Roger Clayton, a healthcare maestro with two decades of unparalleled experience in medical insurance. As the visionary behind Medinscoverage, Roger's mission is to demystify the labyrinth of healthcare coverage, empowering individuals to make well-informed decisions about their well-being. His profound industry knowledge has been the cornerstone in crafting the website's exhaustive resources, offering users indispensable guidance and tools for their healthcare needs.
More Posts